SKIN
Removal and Repair of Skin Lesions
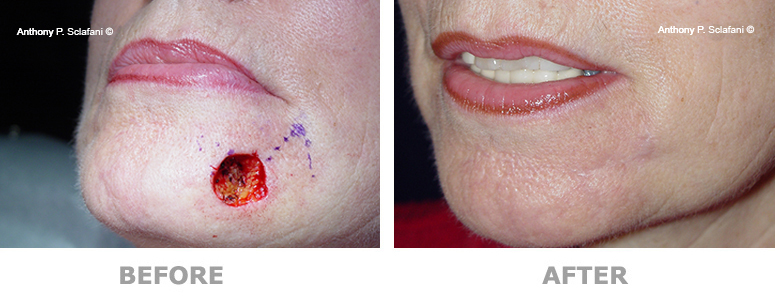
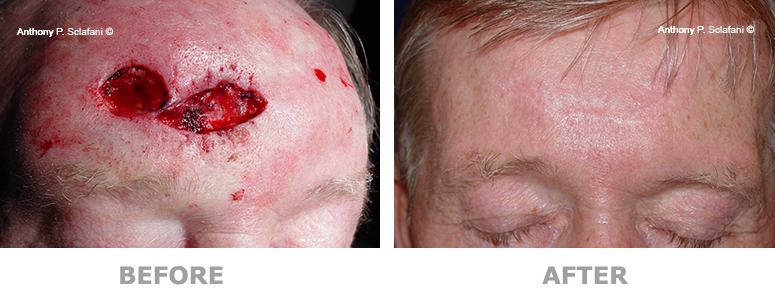
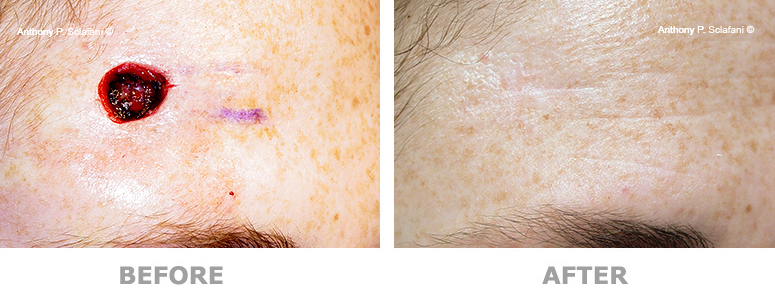
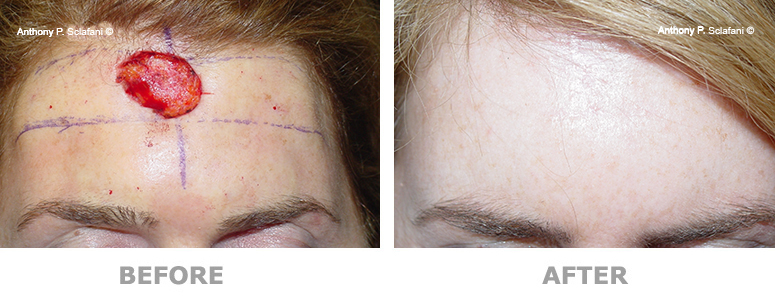
Skin lesions can present as blemishes, or may represent precancerous or cancerous tumors. These may be removed to improve appearance or to remove the potential for cancerous changes. Some lesions can be simply excised and closed.
Repair of Skin Defects Removal of skin lesions and tumors can leave significant deformities. These areas can be reconstructed using a variety of techniques.
Shown here are before (left) and after (right) views of actual patients. Remember, every patient responds differently to surgery, and no one can be certain that he or she will get the results shown. However, these photos will illustrate the changes that are possible with these procedures.













Removal and Repair of Skin Lesions -
Process and Procedure
The Process
Most small benign lesions can be removed in the office; larger or clinically suspicious lesions may be more appropriately treated in an operating room.
The Procedure
Other lesions, if suspicious for cancer, may be removed and immediately examined by a pathologist. The pathologist checks the edges of the lesion to ensure complete removal of the cancer. Should tumor cells be found at the edge, additional tissue can be removed and checked until all tumor has been removed. This is sometimes done in conjunction with a dermatologist.
What to Expect After Removal and Repair of Skin Lesions
DRESSINGS/SUTURES
A small dressing is placed over the scar in the operating room, which can be removed the day after surgery Once removed, an antibacterial ointment is placed over the sutures two to three times daily until the sutures are removed.
Sutures are removed one week after surgery. Some sutures hidden in the hair may be removed somewhat later.
ACTIVITY AFTER SURGERY
In order to allow your tissues to heal properly, we ask that you refrain from brisk physical activity for two weeks. Walking and non-physical activities are allowed, but it is best not to exercise for the first 2 weeks. After the first 2 weeks, aerobics, running, stair climbing, exercise bicycling and treadmills are permitted, but weight lifting (free weights or machines) should not be done until after the end of the third week after surgery. However, once the effects of the anesthetics have worn off, it is not necessary to remain in bed or at home. You may shower the day after surgery, after first removing the dressing. While it is not necessary to cover the sutures, some patients are more comfortable socially if they cover the sutures with a Band-Aid
SWELLING AND BRUISING
Facial swelling is expected and may be more pronounced 24- 72 hours after surgery than it is immediately following the procedure. Sleeping with your head elevated and sitting upright during the day for several days following surgery will help minimize swelling. Most swelling will gradually resolve in 10 days.
Bruising, too, is normal. The bruises on your face may "fall" onto your neck and upper chest before disappearing. Most bruising will resolve in the first 7 days after surgery and may be concealed with makeup beginning the day after surgery (except immediately around the wound). In order to limit bruising and swelling, ice compresses should be applied over the area for the first 24- 36 hours after surgery. Compresses should be applied for 20 minutes at a time, with 20 minutes before reapplying. Also, homeopathic medications Arnica Montana and Bromelain may limit bruising and swelling. This is best started at least 1 week before surgery and continued for 3 weeks; check with your doctor before using these.
BLEEDING
Minimal oozing of blood and tissue fluid along the suture/staple lines may occur for a day or two following surgery. Bleeding that is severe or does not stop with 10 minutes of continuous pressure is rare and should be reported to our office.
PAIN/DISCOMFORT
Most patients experience little pain afterwards; most describe the discomfort as "soreness" rather than "pain", easily controlled with acetaminophen or acetaminophen with codeine.
FOLLOW-UP SKIN CARE
Many skin lesions can be pre-cancerous, and the same general recommendations apply to those circumstances as do to patients with proven skin cancers. Routine follow-up (generally every 6 months, occasionally more frequently) with a dermatologist is recommended for routine skin surveillance.
